In December 2019, the World Health Organisation (WHO) commemorated the 40th anniversary of smallpox eradication. Ironically, later that month the world was introduced to a new epidemic caused by the Novel Coronavirus. At the same time, the WHO’s fight against other epidemics such as the Ebola virus outbreaks in Congo is far from over. As the world becomes smaller in terms of access, the risks associated with a disease outbreak becomes greater.
Every disease outbreak puts our healthcare system in disarray. Not only does it affect the country where it originated, but it also has a far-reaching impact on healthcare systems in other countries. As of today, the coronavirus has reportedly spread beyond China to 16 countries. A visit to a public healthcare facility in Singapore in the last few days shows how the healthcare system is tracking everyone who visits a hospital or a polyclinic – not just patients. Clinicians are also conducting extra screenings. This has ramifications for healthcare systems, that are already strapped with staff shortage.
There are obvious economic ramifications – at least in the short term. Several companies are banning travel to China for their employees, while many manufacturing units in China have had to temporarily shut down. The impact is not restricted to China alone and has the potential to impact global trade and economy.
Every new disease that comes into the limelight also impacts the life sciences industry that has to divert their R&D resources into finding a cure and/or a vaccine for the disease. While winning the race for the first breakthrough can be a huge opportunity for the pharmaceutical company, it also impacts the regular research being conducted to protect us from other deadly diseases.
Unfortunately, we are always one step behind diseases, and we have to first think of cure and containment before we can consider prevention and eradication. As we wait and watch to see how fast the coronavirus epidemic is contained, we must acknowledge the role technology plays in managing epidemics and other disasters. Here are some initiatives:
Detection
One of the success stories to emerge from this disaster is the speed at which the risk of the outbreak was detected. 10 days before the WHO announcement, BlueDot, a healthcare monitoring platform had already detected the epidemic, from intelligence gathered from news reports, disease networks and official sources. The same platform – and a few others – are also predicting the global spread of the virus by mining global airlines ticketing data. This is a reassuring outcome of how technology and human analysis can effectively come together to improve health outcomes.
Research
While the current global concern is the speed of containment of the disease, eventually there will have to be more proactive measures to prevent another outbreak and to even eradicate the disease. To be able to understand the full nature of the pathogen and to come up with a vaccine, it is important that the virus is isolated. Scientists from the Peter Doherty Institute for Infection and Immunity in Melbourne successfully grew the Wuhan coronavirus from a patient sample. While the Chinese authorities had released the genome sequence to help with the diagnosis, this ‘game-changer’ can be potentially used to detect the virus in patients who do not yet display the symptoms and eventually to develop a vaccine. Cutting-edge research in healthcare has always been conducted by such research and pharmaceutical organisations. They have consistently pushed the adoption of new technology in healthcare, especially in their R&D practices.
Management
As mentioned earlier, any outbreak taxes the front-line healthcare providers the most. They have very little time to change their triage and protocols to combat a disease that they have possibly never encountered. This is where clinical decision support systems that can incorporate these new protocols into the workflow comes in handy. Epic, the EHR provider has pushed a software update that does just that. According to Epic, this update was developed in collaboration with biocontainment experts, infectious disease physicians and the US Centers for Disease Control and Prevention (CDCs). Collaborations such as this will be required if we have to devise a global protocol for epidemic management and containment.
There have been several other initiatives during this outbreak that show how different technologies can come together to benefit healthcare, especially to handle a crisis. Technology has always played a huge role in spreading the message in times of disaster, especially in emerging economies – with technologies such as AI, the potential of technology benefitting healthcare increases exponentially.

Authored by attending Ecosystm analysts, Sash Mukherjee (Principal Analyst, Government & Healthcare) and Sid Bhandari (Director, Consulting & Advisory Services)
The recently held AWS Public Sector Summit in Singapore showcased some of the regional AWS implementations, and how organisations are leveraging the Public Cloud differently.
In her keynote address, Teresa Carlson, Vice President, Worldwide Public Sector set the tone for the industry show cases by saying that a successful Digital Transformation (DX) starts from a radical rethinking of how an organisation uses cloud computing technology, people, and processes to fundamentally change business performance.
AWS Empowering the Public Sector
Carlson is clear on what Public Sector organisations must do and where AWS can help them:
- Define what Cloud refers to in the organisation. The first step in bringing about a Cloud First transformation is to be clear on the true definition of cloud computing.
- Create a “Cloud First” policy. To adopt a Cloud First policy, it is imperative to have leaders with a clear vision who really drive technology initiatives forward for all the right reasons like security, cost reduction, scalability, privacy and rapid acceleration of citizen services.
- Focus on Security & Compliance. AWS has global compliance certifications with 200+ services and key features focused on security, compliance and governance. New services such as the use of AI for threat detection have been implemented and are quickly evolving into a mainstream feature.
- Modify your Procurement vehicle. A formal cloud procurement model must be adopted instead of creating ad-hoc processes and a rush to adopt cloud to meet the specific needs of individual departments. AWS has the expertise to assist government IT leaders in selecting the right acquisition approach for their agency.
- Do not ignore Skills Development. Investing in cloud skills development – whether at the central IT level or in the individual business units in the Public Sector – is imperative, as roles evolve and new roles emerge. AWS has over the years offered free courses and industry certifications to Public Sector employees interested in learning the foundations of cloud computing, storage, and networking on AWS to advanced skills courses in emerging technologies such as AI.
Ecosystm Comment:
While cloud may have started off as a means of offsetting CapEx, its role has since evolved into being a major vehicle for DX. Several governments across the world have adopted Cloud First policies to spearhead innovation, increase agility, and improve citizen services. Cloud is increasingly seen as a foundation for many emerging technologies that governments are experimenting with and implementing such as AI, automation, Big Data analytics and Smart Nation initiatives.
The skepticism around Public Cloud security seems to have diminished over the years, with the perception that cloud providers use state-of-the-art technologies to protect their environment and continue to upgrade their security features in the face of new and evolving threats. However, the Ecosystm Cybersecurity study finds that nearly 53% of Public Sector and allied organisations that use Public Cloud feel that the security measures offered are sufficient. Leading cloud providers such as AWS should make it clear that essentially it is a shared responsibility and impress on organisations that the responsibility to secure their own applications and the interface with the Public Cloud ultimately lies with the deploying organisations.
Industry Use Cases
There were several industry use cases presented over the 2 days and it was heartening to see so many Asia Pacific examples of transformation. Tan Kok Yam, Deputy Secretary, Smart Nation & Digital Government Office shared that the key to a successful Smart Nation initiative is to build user-centric services rather than having an agency-centric approach, in his presentation on Singapore’s “The Moments of Life” app. Edwin H. Chaidir, IT Manager at WWF Indonesia presented on how AWS’s machine learning capabilities has helped the organisation to automate identification of specific orangutans in the wild, freeing up resources (money and time) to reinvest in other wildlife protection initiatives.
One of the implementation stories that impressed the Ecosystm analysts was the one shared by Rookie Nagtalon, Consultant for Digital Transformation at the Chinese General Hospital and Medical Center (CGHMC) in the Philippines, where he spoke about how they were able to bring about transformation in their patient life-cycle management. Healthcare in Asia Pacific is a diverse and disparate market with organisations at different levels of IT and business maturity – against a backdrop of different country-level goals and healthcare policies. It was encouraging to hear about a transformation project in a not-for-profit organisation from an emerging economy.
The challenges that healthcare organisations face are unique in many ways:
- Legacy systems that still work and hence there is no business case for replacing them
- Approximately 2/3rd of the IT budget going into running the basics, leaving limited resources for emerging technology adoption and transformation projects
- The shift to value-based healthcare and the need for data-driven insights to support it
- The unpredictability of the workload and the need for an agile IT infrastructure
- Security and compliance mandates that protect patient data and require storage of records over extended periods
Working with these challenges, how does a healthcare organisation bring about Digital Transformation?
Nagtalon’s team was assigned the task to bring about this transformation within a 10-month timeframe.
- The key challenge. An awareness that no one vendor can provide the entire gamut of functionalities required for patient lifecycle management. In spite of recent trends of multi-capability vendors, hospitals need multiple vendors for the hospital information system (HIS), ERP, HR system, document management systems, auxiliary department systems and so on. Each of these vendors have their own development team and infrastructure requirement, which stresses the internal IT resources. DX involving multiple legacy systems requires a step-by-step approach. The challenge is to identify the right systems to start the journey with.
- Vendor selection criteria. The need to find one solution that would enable seamless data sharing across the disparate systems. The vendor selection criteria that were used focused on ease of use and speed especially when working with multiple data sources. In keeping with the industry, the ability of the vendor to support mission-critical applications was put through the filter of what was referred to as ‘Code Blue’.
- The solution choice. A cloud solution that can empower teams and remove worries about the infrastructure. The hospital chose AWS as their transformation partner, who used a system interface blueprint to integrate data from their SAP ERP system, Medcurial’s MeRx HIS, 128 HR system, Canon’s documentation system and multiple diagnostics systems.
- The future roadmap. Enabling the organisation to be a Digital Hospital. The solution was implemented in 7 months and hit the right ROI requirements, reducing billing time and impacting the bottom line in terms of both recovery and revenue. It has created the base foundation for future plans such as device integration and the provider is well set on its journey of Cloud, IoT and Robotics.
Ecosystm Comment:
Nagtalon raised an important point when he was asked the key reason for the success of the project – executive buy-in. Transformation projects work best when it is enterprise-wide and senior management sponsorship is a must to enable that. However, he also mentioned humorously that he had become extremely unpopular during the implementation. This is where a centre-of-excellence with ‘champions to the cause’ from each key department helps. Organisations should look to engaging with the stakeholders early and to get their buy-in as well as the executive’s.
AWS’s marketing message to healthcare providers includes allowing them to focus on their mission and create their differentiation, and enabling them to incorporate new and emerging technologies. This implementation certainly ticked those boxes. What was particularly positive was the big thumbs up the AWS implementation team received. Organisations will increasingly partner with platform providers in their transformation journeys and implementation capabilities and best practice guidance will be the key differentiators for vendors.
Globally, the HealthTech innovation ecosystem has many startups working at the intersection of IoT and AI to solve some of the tough problems faced by patients and other stakeholders in the healthcare space. Several factors have led to a proliferation of a class of devices in the health, fitness and wellness space – such as, miniaturisation of sensors, advancements in microcontroller design and power management, low cost and flexible circuit design The ubiquitous availability of smartphones and always-on connectivity has enabled real-time access to cloud-based AI capabilities to transform IoT data into meaningful insights that can be used anywhere and anytime.
The key objective of healthcare provision is to engage the multiple stakeholders involved within an ecosystem to deliver better and holistic clinical outcomes.

The Key Challenges to Widespread Stakeholder Acceptance
Despite the promises and great potential of IoT and AI in the healthcare industry, there are major gaps in adoption by stakeholders, especially clinicians. I believe there are three main reasons for the gap:
-
The Principle of Conservatism in Medicine
The basic premise of medicine is “Do NO Harm”. Due to the relative newness of both devices and apps, there is only a small body of knowledge and precedence for a clinician. This is too small to take a risk with using “new” data to make decisions, even though the new data may be better than other available “time-tested” options on hand.
Clinical diagnosis is based on years of medical training, time-tested knowledge and practice and clinician “Gestalt”. More often than not, the way an AI system performs the predictions is not fully understood by the clinician. Because of the relatively new field, any new AI-based prediction system will need to establish its credibility that it will NOT do any harm to the patient. Clinicians value their ability to do the right thing for the patient more than anything else.
Establishing the trust between the clinician and the black-box algorithm is critical for any successful adoption.
-
Features vs. Function
There is a lack of a common language and understanding between clinicians and technologists, especially when it comes to what “innovation” means for the other party. For a technologist, innovation lies mostly in the features and capabilities of the technology. Their mindset is that innovative technology can be easily adapted to healthcare, similar to the way mobile phones have been adopted by consumers. Their belief is that people and practices will change quickly when presented with better technology and insights. For a technologist, innovation is what transforms a practice in leaps and bounds.
For a clinician, innovation is incremental to start with, and it evolves with time. There is a widely-held belief that if a new technology is not easy to understand, then it probably will not be good. Features and capabilities do not mean much to them. Innovation MUST be simple to understand, reliable, repeatable and MUST solve a problem that they cannot solve by themselves. The arguments in the public domain whether or not AI will replace clinicians adds to the skepticism.
-
Evidence through Clinical Trials
Perhaps the biggest factor of all is that clinicians demand evidence of safety and efficacy of new technology through the lens of time-tested processes of randomised clinical trials. Unless there is evidence created by the technologists through well-designed and robust clinical trials, adoption of new technology will be a hit and miss. Technology companies interested in transforming healthcare should have a solid understanding of the clinical trials process and should create adequate scientific evidence to positively influence clinicians.
The most important aspect of gathering clinical evidence is to identify the relevant data for decision making. Many clinicians do not readily utilize the data collected from connected healthcare devices into their diagnosis and decision processes due to the lack of connections between data and clinical practice. While 10,000 steps a day might be a good benchmark for exercising right, that number means nothing if it is not connected to a clinical decision framework.
The Way Forward for Stakeholder Adoption
Healthcare leaders predict that the implementation of healthcare IoT and AI solutions on a scale will transform their industry. The next few years will see more interconnected IoT devices and reliable applications based on deep learning. To achieve adoption and impact of new technology, the innovators and healthcare stakeholder ecosystem leaders should address the need for trust and evidence. Real World Evidence and Randomised Clinical trials are effective ways to bridge the gap and to establish a common framework to address the user adoption issue.
Arun Sethuraman, Principal Advisor MedTech, Ecosystm is also the founder and CEO of Crely Healthcare, a MedTech startup based in Boston and Singapore. Infection of the surgical site, post-surgery, if not detected and treated early, leads to high incidence of mortality in patients, poor health outcomes, poor patient experience, higher healthcare costs, and loss of reputation and reduced profitability for healthcare providers. Crely’s mission is to provide an early warning and clinical decision support system for surgical site infections (SSI), post-surgery. Crely generates an early warning of SSI by algorithms based on biomarker data collected from patients using an IP-protected, secure, non-invasive, continuously wearable, clinical grade medical device.

There is no argument that the healthcare industry is ripe for Digital Transformation, especially because the needs and concerns of the industry have remained essentially consistent over the last few decades, in spite of tremendous technological advancements. Healthcare organisations have access to higher volumes of data than ever before. While a decade ago healthcare organisations were at a data creation stage, they will now shift focus on data management, extracting intelligence out of the data collated, and the use of that intelligence to transform their organisations and the industry, as a whole. So, what can the industry expect in 2019?
- India will Receive a Lot of Attention from Technology Vendors
At the turn of this decade, there was a plethora of healthcare IT vendors, driven by investments in the Affordable Care Act in the US. The industry has since become far more consolidated. A similar situation will open up in the Indian market. What is popularly being termed as ‘Modicare’ is narrower in scope and has a long way to go in terms of policy as well as planning. However, it will create a ripple effect and get vendors – especially the smaller ones – very interested in India in 2019. Every large global insurance company has a presence in India, attracted by the population base. It will be similar for healthcare technology vendors. - CX will go Beyond Managing Patient Experience to Providing Personalised Healthcare
Improving customer experience (CX) is a key objective for most healthcare organisations. This has been compounded by how technologically savvy people have become over the years. Patients often do their own research before they even visit their doctors. While most physicians consider this a bit of a nuisance, it is increasingly going to be the way forward. Patients are also expecting better experience, when it comes to access of timely alerts and information, education, and access to their reports. Healthcare organisations will eventually go beyond patient experience to personalised healthcare and deeper customer engagements. While this will become most apparent for chronic disease management, it will go into spaces such as predicting patient risk over the next few years. - Operations will Lead Investments in IoT ….
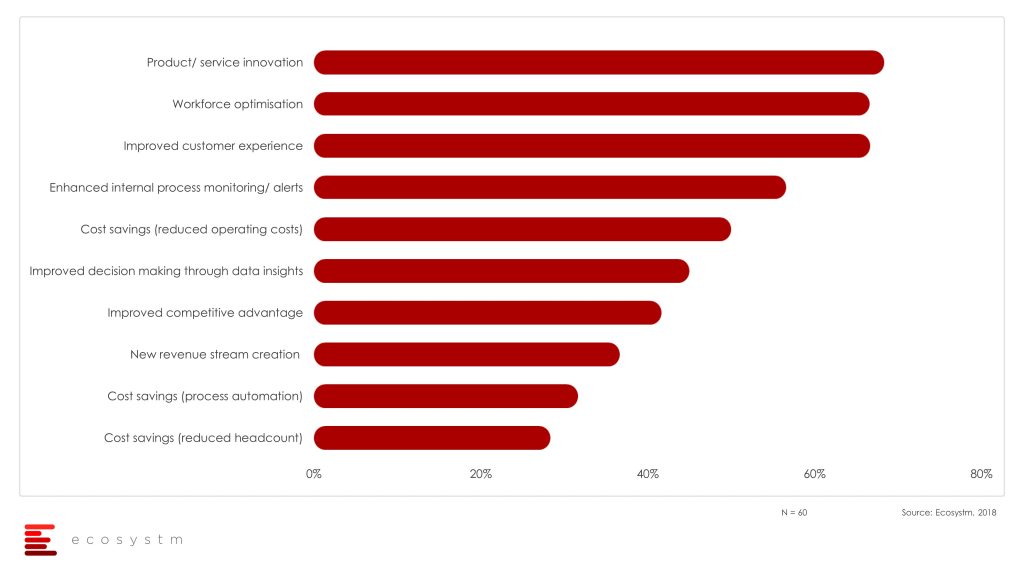
The global Ecosystm IoT Study reveals that of the healthcare organisations that have embarked on their IoT journeys, 2/3rd are still at the evaluation stage. What then are the drivers for healthcare organisations to adopt IoT? The top three drivers tell us that the key stakeholder is not the clinical departments, but Operations. Struggling with the workforce constraints, IoT is deemed as the technology that will allow better optimisation and innovative ways of providing customer care to improve patient experience. Internal process monitoring emerges as a key driver, in an industry where medical error monitoring and reporting is an important mandate.
- But Diagnostics will Sneak in as the Gateway to AI Investments
The two key areas where AI will see the easiest application in healthcare are in diagnostics and clinical decision support. Diagnostics using machine learning, predictive analytics and pattern recognition can be utilised effectively for clinical decision support. IoT sensor analytics, image analytics and machine learning, will start getting used to improve the efficiency and the reliability of the diagnostic processes. Algorithms can be applied to large data sets, especially in auxillary departments such as Radiology, Pathology and Cardiology, to augment clinician inputs. - Security will Play Spoilsport for Investments in Clinical Intelligence
As health management software gets more and more networked, security has to keep pace with the functional aspects of deployed applications and implementing organisations will ignore this aspect as their peril. The data breach in Singapore is not by any means an isolated episode, and especially mature economies with well-defined health data protection laws will pause before using cloud options for clinical data management. This is true across industries as my colleague points out in the cloud predictions for 2019.